New understanding of what causes "chemobrain," or chemotherapy-related cognitive impairment (CRCI), may eventually lead to treatment or even prevention, say neuroscientists.
The new insights come from studies in postmortem human frontal lobe tissue and from a mouse model of methotrexate-induced neurologic dysfunction.
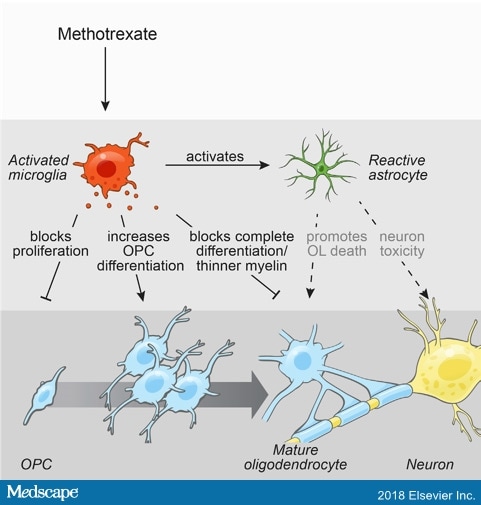
They show that methotrexate chemotherapy triggers the brain's immune response, creating inflammatory microglia cells. This in turn triggers neurotoxic reactivity in astrocyte cells that support synaptic connectivity, causing dysregulation of oligodendrocyte cells involved in myelination and homeostasis.
Methotrexate induces persistent tri-glial dysregulation (Cell. 2019;176:43-55).
The good news? The team showed that an experimental drug depleted inflammatory microglia, normalized cell activity, and restored cognitive function in the mouse model, say Michelle Monje, MD, PhD, associate professor of neurology and neurologic sciences at Stanford University School of Medicine in Palo Alto, California, and colleagues.
In their study, they used the colony-stimulating factor 1 receptor (CSF1R) inhibitor PLX5622. They note that similar agents are currently in clinical trials for other indications.
The study report was published online December 6 in Cell.
"These findings indicate that methotrexate chemotherapy exposure is associated with persistent tri-glial dysregulation and identify inflammatory microglia as a therapeutic target to abrogate chemotherapy-related cognitive impairment," the investigators write.
"It's an exciting moment," said Monje in a statement from Stanford. "If we understand the cellular and molecular mechanisms that contribute to cognitive dysfunction after cancer therapy, that will help us develop strategies for effective treatment. There's real hope that we can intervene, induce regeneration, and prevent damage in the brain."
Clinical trials into interventions are expected to being within the next 2 years, she said.
Monje said she suspects this type of complex dysfunction may underlie other cognitive disorders seen in demyelinating diseases, such as multiple sclerosis. "I think that is probably more the rule than the exception," she commented.
Major Cause of Morbidity
The American Cancer Society has estimated that the number of cancer survivors in the United States will increase from 15.5 million in 2016 to 20.3 million by 2026. "Thus, CRCI represents a major source of morbidity during and after cancer therapy and a great unmet need to be addressed," the researchers point out.
In an interview, Monje emphasized that chemobrain is real, and extremely debilitating. Most studies show it can last for weeks, months, or even decades following chemotherapy, she said.
Patients describe chemobrain as a "mental fog" that leaves them unable to focus, multitask, or process information at a normal speed. It can also impair fine motor and executive functions, often creating anxiety, she said.
"I can't tell you how many cancer patients are affected long term, but the majority of cancer survivors have some degree of cognitive impairment," she told Medscape Medical News. "It's important to recognize how real this is and that there are people working to understand it and treat it."
It's important to recognize how real this is. Dr Michelle Monje
Children who undergo chemotherapy are especially vulnerable, said Monje, whose practice consists of adult survivors of childhood cancers, such as leukemia, sarcoma, and brain cancer. "Methotrexate is not only hitting cognitive flexibility and adaptability but also brain development," she pointed out.
Methotrexate, an antimetabolite agent commonly used to treat a range of cancers, is "a particularly bad chemotherapy for cognitive impairment," noted Monje.
"When I ask my patients whether they have difficulty paying attention, multitasking, or remembering things, there is very frequent cognitive impairment. Many patients, even those who are high functioning, don't realize what is happening to them, and many oncologists don't realize either and don't offer these patients symptomatic therapy," she said.
Central nervous system stimulants that improve concentration "can be very useful in the clinical setting," said Monje. There is also some evidence for the efficacy of anti-Alzheimer's medications to improve memory.
"Oncologists need to ask patients about attention and memory, because there are symptomatic therapies that neurologists can provide," pointed out Monje. "I have taken care of people who went on to get a PhD."
Effects on Myelin Microstructure
The study of postmortem frontal lobe tissue showed that in children and young adults treated with multiagent chemotherapy, oligondendrocyte precursor cells (OPCs) involved in myelination were significantly depleted for at least 6 months compared to age-matched control persons who had not received chemotherapy (4150 ± 876 cells/mm3 vs 14,893 ± 2063 cells/mm3).
OPCs contribute new myelin-forming cells to white matter, which is heavily myelinated, the researchers explain. This is "where the constellation of symptoms that make up CRCI tend to localize," they point out.
The study also showed that methotrexate exposure was associated with persistent activation of inflammatory microglia and subsequent reactivation of astrocytes, another major neural cell type that promotes neural crosstalk by supporting synaptic connectivity. The researchers explain some of this in cartoon form in this video.
In the mouse model of methotrexate CRCI, the investigators observed a similar depletion of white matter OPCs. Transmission electron microscopy showed a substantial decrease in myelin sheath thickness at 4 weeks and 6 months post treatment compared to control mice.
When OPCs were transplanted from chemotherapy-naive mice into mice exposed to methotrexate, increased OPC differentiation was also observed. "These data indicate that methotrexate chemotherapy is associated with lasting changes to myelin microstructure," the researchers say.
Behavioral changes consistent with persistent cognitive deficit following methotrexate exposure were also observed in treated mice compared to control mice. These changes included decreased forepaw swing speed, increased anxiety, and decreased ability to discriminate between novel and familiar objects 6 months post treatment.
"Collectively, these data demonstrate that this mouse model exhibits behavioral deficits similar to the symptoms humans experience after chemotherapy," Monje and colleagues say.
Treatment with the CSF1R inhibitor PLX5622 depleted inflammatory microglia and normalized OPC function, "restoring myelin microstructure and cognitive behavior," the researchers note.
"We picked one that works, but are there others that are advantageous?" asked Monje. "As more is understood about the molecular mechanisms mediating how methotrexate causes microglial inflammation and how microglial activation disrupts these important intercellular interactions, it is hoped that further regenerative strategies will be developed," she told Medscape Medical News.
"We describe the cellular components, but we have a lot of work to do to understand the molecular mechanisms. We need microglia to come back in a functional way, and understanding how molecular mechanisms result in dysfunction will highlight additional therapeutic interventions."
Among the many questions yet to be answered is that concerning the timing of microglial depletion, noted Monje.
"We did this right after chemotherapy [in the current study], but can we deplete microglia long after chemo exposure and still rescue patients from the cognitive deficits? Or is there a point of no return, after which you can't rescue the myelin anymore? We don't know this yet. But I'll wager a guess there will be some intervention possible even in the long term," she said.
The study was funded by a number of research foundations, including the California Institute for Regenerative Medicine. Monje and coauthors have disclosed no relevant financial relationships.
Cell. Published online December 6, 2018. Abstract

Δεν υπάρχουν σχόλια:
Δημοσίευση σχολίου